Sciatica: What is it and how do we treat it?
- Jonathan Brown
- Nov 2, 2023
- 4 min read
Updated: Nov 3, 2023

This is a deep dive on sciatica; the causes for it, what some of the terms generally associated with it mean and how we successfully treat it in clinic.
Classed as pain in the lower buttock, hamstring, lower leg or foot, sciatica can, at its worst be excruciating and at its best a mild annoyance. It is estimated that around 5-10% of lower back pain is as a result of sciatica.
To understand what it means to have sciatica, we first need to delve a little into the anatomy of what the sciatic nerve is and where it stems from/to.
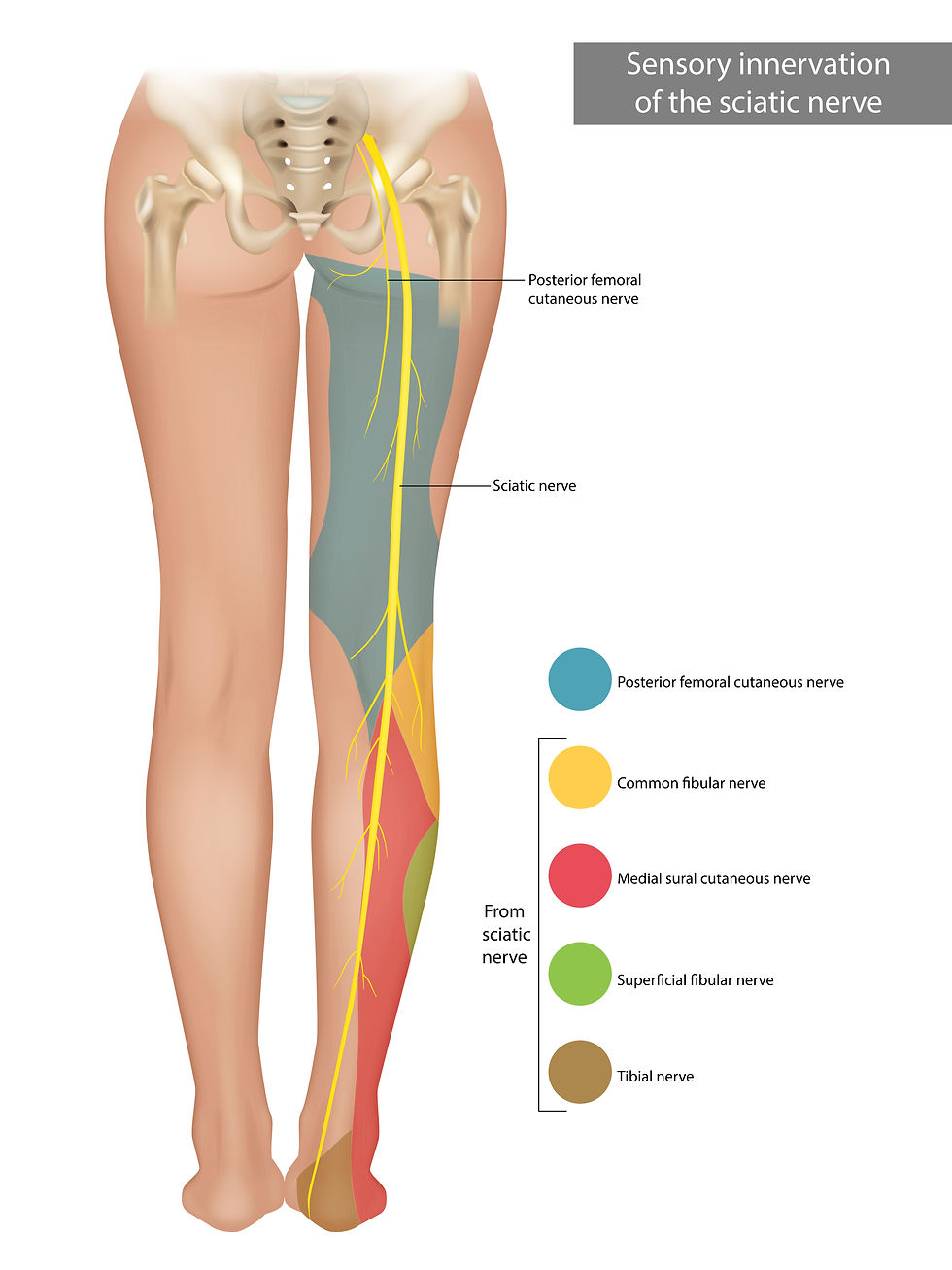
The sciatic nerve is the body’s largest and longest nerve; running from the lower back, through the buttocks and down each leg; It originates from L 4/5 and S 1,2&3 and has two major nerves and many sub-branches that fan out as it leaves the spine and works its way down the leg.
The common fibular nerve
The tibial nerve
Sub branches of the above; the superficial and deep fibular nerves, medial sural cutaneous nerve and medial calcaneal branches all connect to the sciatic nerve and thus are implicated in the pain/numbing/irritation that comes with sciatica symptoms.
*The posterior femoral nerve can also contribute to sciatica type symptoms but isn’t directly linked to the sciatic nerve but does share a common innervation site.
Worse case scenarios of sciatica are the result of genuine compression of the spinal chord or the nerve roots that exit the spine. This can occur via:
Herniated or slipped disc. This occurs when soft inner material of the spinal disc pushes out through an opening or rupture, putting pressure on the adjacent sciatic nerve.
Spinal Stenosis or the narrowing of the spinal canal (inside your spine) can lead to compression of the sciatic nerve. This particular circumstance may or may not require surgery.
Epidural abscess; a rare but serious infection. The collection of pus or fluid at the site of infection can compress the sciatic nerve and require immediate medical attention.
Epidural tumours; another rare but serious complication growing nearby can also result in compression of the sciatic nerve.
Pain in these scenarios are sometimes debilitating. The compression on the nerve root or the spinal chord itself is acute and most patients find almost no position comfortable. In the very worst case scenarios surgery is the only way to free the body from extreme compression of the nerve or spinal chord. In many instances, surgery can provide incredible relief and the recovery time post surgery is well worth the trauma of going under the knife.
But even some acute cases of spinal stenosis or milder herniation diagnosed via scans don’t need surgery. There is a lot that can be done to reduce and completely eradicate these symptoms.
One other hardware related cause for sciatica or nerve compression is disc degeneration. Known as degenerative disc disease.
This is NOT to be confused as an actual disease in the way that we normally view diseases, it is simply the culmination of wear and tear on the joints/intervertebral discs over time. The inflammation of these scenarios or narrowing of joints can cause some chronic cases of sciatica. They generally do not require surgery. In cases of disc degeneration we need to tackle the inflammation at the sites of mild compression/irritation of the nerves whilst desensitising and increasing ranges of movement.
Thankfully most sciatica symptoms are much milder and more often, NOT caused by compression of the spine.

The compression/irritation of the nerves can come from any number of structures; including muscles, tendons, ligaments or other connective tissue.
Your muscles etc are not like the anatomy drawings where they sit stationary. You are a moving body and as such, your tendons, ligaments and muscles are constantly shifting, lengthening and shortening; This is all normal. Your subconscious is also constantly receiving, processing and reacting to immeasurable quantities of information from proprioceptive receptors, reactions to chemicals, hormones, nutritional ingestion or emotional states. All of which have to be processed and reviewed in a microsecond for safety and danger. And all of which can have an affect on how your musculoskeletal system works.
Much like our conscious perception of things, our subconscious can also process certain information incorrectly or hyper-sensitively.
Sometimes, what should be seen as normal proprioceptive information that is received by your subconscious is processed as dangerous or potentially harmful to you. Your brain will adjust or adapt around these perceived threats and from a movement perspective, may prevent you from doing something, or could move you away from a threat.
This can result in muscles, tendons or ligaments tightening, preventing you from moving as efficiently. Or from a spinal perspective, can result in joints locking up to “protect” you from information perceived to be a threat.
Then through the pursuit of normal movement against a backdrop of restriction, can cause mild compression or irritation of the nerve.
The classic representation of this is known as Piriformis Syndrome. Which is where the external rotator muscles at the rear of the hip (including the piriformis) become hypertonic and tight. Just like the example given above where movement is still required; these muscles that no longer have the capacity to move efficiently, cause compression or irritation of the nerve.
This type of scenario is representative of most acute and chronic sciatica. There isn’t any real injury or damage to note, just the end result of inefficient movement brought on by perceived threats.
How do we treat this form of sciatica in clinic?
In this milder scenario, treatment takes a multi-pronged attack.

Firstly, if there is some level of inflammation to tissue/nerves as a result of inefficient mechanics, we treat this through the application of photobiomodulation laser therapy and added supplemental antioxidants.
Secondly the information that is being processed as dangerous which is causing your subconscious to alter your movement efficiency needs to be identified and desensitised. This is the most important part of treatment as it directly addresses the WHY you have pain and is achieved through the use of functional neurology in the form of P-DTR.
Lastly when the subconscious no longer sees something, for example a stretch to a ligament, as dangerous, the nervous system allows muscles/tendons/ligaments and joints to move in their full ranges. We help to increase and maintain those increases in movement potential by securing movement patterns neurologically.
Combining all of these methods of treatment is part of the blueprint Four Step-Treatment Process utilised here.




Comments